Red Light Therapy for Psoriasis: Can It Help?
Psoriasis is a chronic skin condition that affects millions of people worldwide, causing red, scaly patches that can be uncomfortable and sometimes painful. Living with psoriasis often means navigating flare-ups, managing symptoms, and seeking reliable information about the best ways to care for your skin.
This article is here to provide you with clear, factual insights about psoriasis, including proven treatment options and the facts about Red Light Therapy. While there’s growing interest in Light Therapy approaches, it’s important to understand straight away that Red Light Therapy is not a cure or treatment for psoriasis. Instead, we'll talk about some medically recognized strategies and what current research says about how Light Therapy may affect skin affected by psoriasis.
What Is Psoriasis?
Psoriasis is a long-lasting, non-contagious skin condition that speeds up the life cycle of skin cells. Normally, skin cells grow and shed gradually, but with psoriasis, this process happens much faster—sometimes in just a few days. As a result, skin cells build up on the surface, forming thick, red patches covered with silvery scales. These patches can appear anywhere on your body, but they’re most commonly found on the scalp, elbows, knees, and lower back.
Common Symptoms and How Psoriasis Affects the Skin
The symptoms of psoriasis can vary from person to person, but the most common signs include:
-
Raised, red patches of skin covered with silvery-white scales
-
Dry, cracked skin that may bleed
-
Itching, burning, or soreness around affected areas
-
Thickened, pitted, or ridged nails
-
Swollen and stiff joints (in some cases, leading to a related condition called psoriatic arthritis)
Psoriasis can range from mild, with just a few small patches, to severe, covering large areas of the body. Flare-ups can be triggered by various factors, including stress, infections, skin injuries, or certain medications.
Types of Psoriasis
There are several types of psoriasis:
-
Plaque Psoriasis: The most common form, accounting for about 80-90% of cases. It appears as raised, inflamed red patches covered with silvery scales.
-
Guttate Psoriasis: Characterized by small, drop-shaped spots, often triggered by bacterial infections like strep throat. It’s more common in children and young adults.
-
Inverse Psoriasis: Appears as smooth, red lesions in skin folds such as the armpits, groin, or under the breasts. These areas are often irritated by rubbing and sweating.
-
Pustular Psoriasis: Marked by white, pus-filled blisters surrounded by red skin. This type can be localized to certain areas or cover most of the body.
-
Erythrodermic Psoriasis: A rare but severe form that causes widespread redness and shedding of the skin. It can be life-threatening and requires immediate medical attention.
Causes and Risk Factors
Psoriasis is believed to be an autoimmune condition, which means your immune system mistakenly attacks healthy skin cells. This immune response leads to inflammation and the rapid production of new skin cells.
While the exact cause of psoriasis isn’t fully understood, several factors are known to increase your risk of developing the condition. Genetics play a significant role—if you have a family member with psoriasis, your chances of experiencing it are higher.
An overactive immune system is also a key factor, as it mistakenly targets healthy skin cells and speeds up their production.
Additionally, various environmental triggers can contribute to the onset or worsening of symptoms. These triggers include infections, skin injuries, stress, smoking, heavy alcohol use, and certain medications.
Psoriasis is not contagious, so you can’t catch it from someone else or pass it on through physical contact.
Living with psoriasis can affect more than just your skin. The visible symptoms can lead to self-consciousness, embarrassment, and social withdrawal. The itching and discomfort can disrupt sleep and daily activities. In some cases, people with psoriasis are at higher risk for other health conditions, such as heart disease, diabetes, and depression.
Proven Treatments and Management Strategies for Psoriasis
Managing psoriasis effectively often requires a combination of medical treatments and lifestyle adjustments. Because psoriasis is a chronic condition with no known cure, the goal of treatment is to reduce symptoms, control flare-ups, and improve your overall quality of life.
Medically Approved Treatments for Psoriasis
Topical Treatments
Topical treatments are usually the first line of defense for mild to moderate psoriasis. These medications are applied directly to the skin and work by reducing inflammation, slowing down skin cell growth, and relieving discomfort.
-
Corticosteroids: These anti-inflammatory creams or ointments are commonly prescribed to reduce redness, swelling, and itching. They’re effective for most people, but long-term use can thin the skin or cause other side effects, so they’re often used in cycles or for short periods.
-
Vitamin D Analogues: These synthetic forms of vitamin D, such as calcipotriene, help slow the growth of skin cells. They’re often used in combination with corticosteroids for better results.
-
Topical Retinoids: Derived from vitamin A, these help normalize DNA activity in skin cells and reduce inflammation. They can cause skin irritation, so it’s important to use them as directed.
-
Coal Tar: One of the oldest treatments for psoriasis, coal tar helps reduce scaling, itching, and inflammation. It’s available in shampoos, creams, and bath solutions, but its strong odor and potential to stain clothing can be drawbacks.
-
Calcineurin Inhibitors: These creams, such as tacrolimus and pimecrolimus, are sometimes used for sensitive areas like the face or skin folds. They work by suppressing the immune response that triggers psoriasis symptoms.
UV Phototherapy
A type of phototherapy, or light therapy, uses specific wavelengths of ultraviolet (UV) light to slow the rapid growth of skin cells. This treatment is typically recommended for moderate to severe psoriasis or when topical treatments aren’t effective.
-
UVB Phototherapy: This involves exposing the skin to controlled doses of ultraviolet B light. UVB slows down the growth of affected skin cells and can lead to significant improvement over time. Treatments are usually done in a medical setting, but home units are available for some patients.
-
PUVA Therapy: PUVA combines a drug called psoralen (taken orally or applied to the skin) with exposure to ultraviolet A (UVA) light. Psoralen makes the skin more sensitive to UVA, enhancing the treatment’s effectiveness. PUVA is generally reserved for severe cases due to potential side effects, including an increased risk of skin cancer with long-term use.
You may be wondering: wait, didn't you say Red Light Therapy can't treat psoriasis? Well, Red Light Therapy is completely different from UV Light Therapy. While UV Light Therapy uses ultraviolet wavelengths to slow the growth of skin cells and is a medically approved treatment for psoriasis, Red Light Therapy uses visible red or near-infrared wavelengths that do not contain ultraviolet rays.
UV light can alter skin cell behavior and is specifically chosen for its ability to target the immune response in psoriasis. In contrast, Red Light Therapy does not cause the same cellular changes and does not have the same effects on skin cell turnover or immune activity.
Because of these fundamental differences, Red Light Therapy is not considered a treatment for psoriasis and should not be confused with the UV-based phototherapy methods prescribed by healthcare professionals.
Systemic Medications
For people with moderate to severe psoriasis or those who don’t respond to topical treatments and phototherapy, systemic medications may be prescribed. These drugs work throughout the body to target the underlying immune response.
-
Oral Medications: Drugs like methotrexate, cyclosporine, and acitretin can help control inflammation and slow skin cell production. Each has its own set of potential side effects, so regular monitoring by a healthcare provider is essential.
-
Injectable Medications: Some systemic treatments are given by injection, either under the skin or into a vein. These are often used for severe or stubborn cases.
Biologic Drugs
Biologics are a newer class of medications that target specific parts of the immune system involved in psoriasis. They’re usually prescribed for moderate to severe cases, especially when other treatments haven’t worked.
-
How Biologics Work: These drugs are made from living cells and are designed to block certain proteins (like TNF-alpha, interleukin-17, or interleukin-23) that drive inflammation in psoriasis. By targeting these pathways, biologics can significantly reduce symptoms and improve skin appearance.
-
Administration and Monitoring: Biologics are given by injection or intravenous infusion, often every few weeks. Because they affect the immune system, they can increase your risk of infections, so regular check-ups are necessary.
Lifestyle Changes and Self-Care Tips
While medical treatments are crucial, lifestyle changes and self-care can make a big difference in managing psoriasis and reducing flare-ups.
-
Moisturizing: Keeping your skin well-hydrated helps reduce dryness, itching, and scaling. Use fragrance-free, gentle moisturizers and apply them after bathing to lock in moisture.
-
Stress Management: Stress is a known trigger for psoriasis flare-ups. Practicing relaxation techniques such as deep breathing, meditation, yoga, or spending time on hobbies can help you manage stress more effectively.
-
Avoiding Triggers: Identifying and avoiding personal triggers—such as certain medications, skin injuries, infections, or harsh skin products—can help minimize flare-ups.
-
Diet and Exercise: While no specific diet cures psoriasis, maintaining a healthy weight and eating a balanced diet rich in fruits, vegetables, lean proteins, and whole grains can support your overall health. Some people find that reducing alcohol intake or avoiding certain foods helps their symptoms. Regular exercise not only improves physical health but also helps manage stress.
Light Therapy and Psoriasis: What Does the Research Say?
Light Therapy is a broad term that refers to the use of specific wavelengths of light to address various health and skin concerns. In the context of psoriasis, the most established and medically approved form is UV Light Therapy, particularly UVB phototherapy. This treatment has been used for decades and is supported by strong clinical evidence. UVB Light Therapy works by exposing the skin to controlled doses of ultraviolet B light, which slows the rapid growth of skin cells and helps reduce inflammation.
For many people with moderate to severe psoriasis, UVB phototherapy can significantly improve symptoms and is often recommended when topical treatments are not effective. Another form, PUVA therapy, combines UVA light with a medication called psoralen to enhance the skin’s response to the light, but it is generally reserved for more severe cases due to potential side effects. It’s important to note that tanning beds are not a safe or effective substitute for medically supervised UV Light Therapy. Tanning beds primarily emit UVA rays, which do not provide the same therapeutic benefits as UVB phototherapy and can increase your risk of skin cancer and other skin damage.
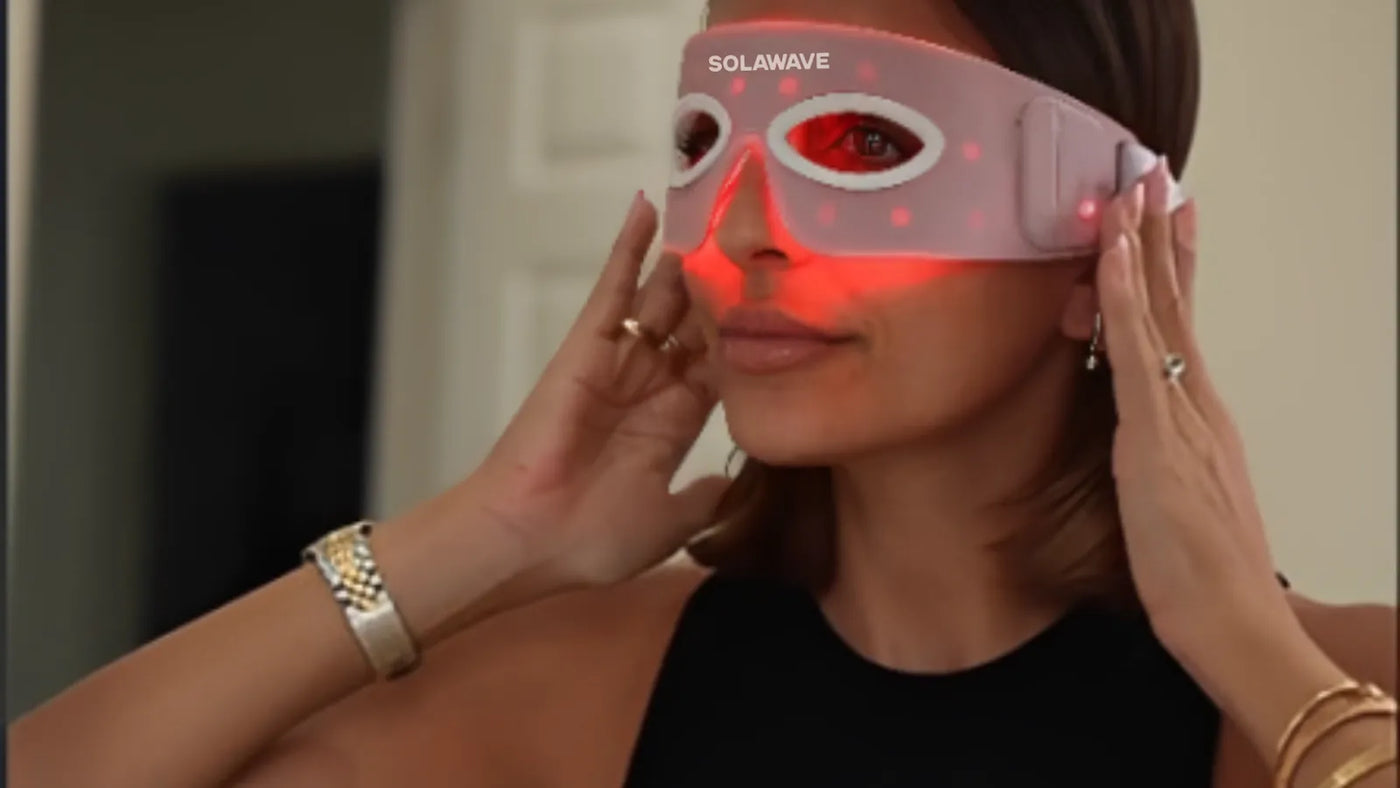
In contrast, the types of Light Therapy commonly used for general skincare—such as Red Light Therapy, Near-Infrared Light Therapy, Blue Light Therapy, and Amber Light Therapy—operate at different wavelengths and do not include ultraviolet rays. These therapies are popular for their potential to combat signs of skin aging, reduce inflammation, and improve overall skin appearance. However, they do not affect skin cell turnover or immune system activity in the same way that UV Light Therapy does. This is a crucial distinction, as the effectiveness of UVB phototherapy for psoriasis is directly related to its ability to target the underlying immune response and abnormal skin cell growth.
When it comes to Red Light Therapy for psoriasis, research is still in its early stages. A few small studies have explored whether Red Light Therapy might help with inflammation or skin healing, but the results are limited and inconclusive. There is currently no strong evidence to support Red Light Therapy, Near-Infrared Light Therapy, Blue Light Therapy, or Amber Light Therapy as effective treatments for psoriasis. These forms of Light Therapy are not approved by medical authorities for this purpose, and they should not be considered substitutes for proven therapies like UVB phototherapy.
Conclusion
Psoriasis is a complex skin condition, but there are proven treatments available that can help you manage symptoms and improve your quality of life. While Red Light Therapy and other forms of Light Therapy are gaining attention, it’s important to remember that Red Light Therapy is not a cure or treatment for psoriasis. For the most effective care, always consult with your healthcare provider to develop a treatment plan that’s right for you. If you’re seeking more information or support, consider reaching out to trusted medical organizations or your dermatologist for guidance and resources tailored to your needs.
Disclaimer: This article is intended for informational purposes only and should not be interpreted as medical advice or guidance. Always seek medical advice and care from a trusted healthcare professional.
Sources:
-
Topical Calcineurin Inhibitors (TCIs) - National Eczema Society
-
Phototherapy: PUVA - American Osteopathic College of Dermatology (AOCD)